In the past two years the state accumulates the highest number of new HIV-positive diagnoses of any state in the United States. From 2015 to 2019 some 35 babies acquired the virus through the mother’s womb, also one of the highest rates in the country. Now cases of gonorrhea, chlamydia and syphilis have increased.
HIV is no longer a radical threshold between life and death with the advance of anti-HIV drugs and increasingly potent antiretrovirals for those infected, but in Florida, which now ranks first in the nation for new cases, including among newborns, the spike in other sexually transmitted diseases is becoming a silent health nightmare.
In a worst-case scenario of new infections, in the last five years (2015 to 2019) some 494 babies born in Florida were perinatally exposed to HIV, of which 35 (an average of nine per year) acquired the virus through the mother’s womb, the highest number of cases in the United States, according to the state Department of Health.
But for the first time in the history of the HIV epidemic, there were no diagnoses of the perinatally acquired virus in Florida in 2019, considering that in 2018 about eight babies tested positive at birth, according to the Florida State HIV Epidemic Plan 2020 reports reviewed by the ITEMP Project.
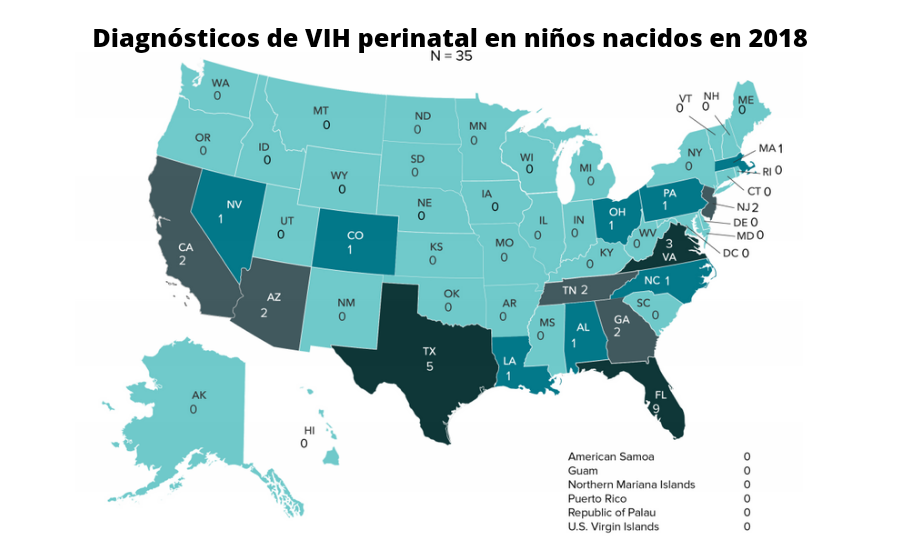
Data from the Center for Disease Control and Prevention (CDC) are bleaker for Florida when it comes to the category of perinatal transmission of HIV to newborns, which generally account for less than 1% of cases nationwide.
With nine and three cases, respectively, Florida and Texas achieved the highest number of virus infections attributed to perinatal transmission in newborn infants during 2018, while in 2017 Florida led the table with nine diagnoses.
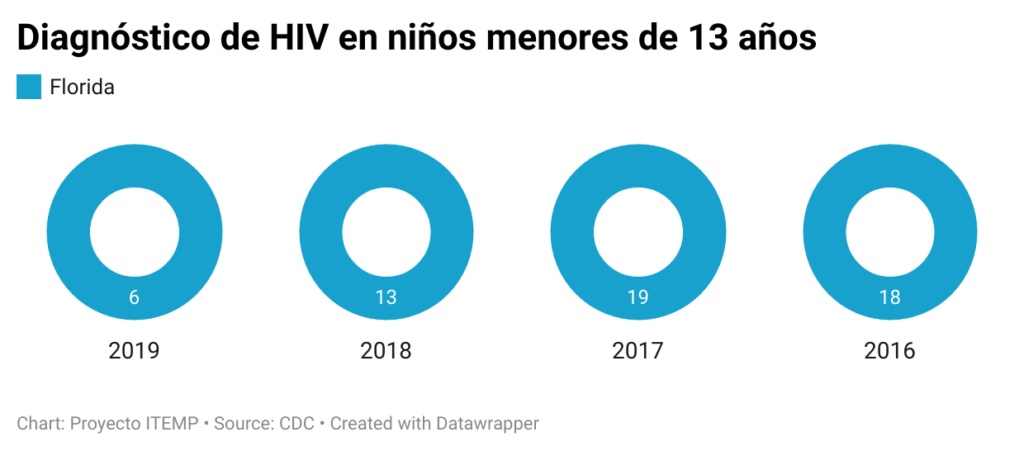
An annual CDC report says that in 2019 about six children in Florida were diagnosed positive for HIV, trailing only Georgia with 10 new cases that year for the top spot nationally.
The Florida Department of Health and CDC did not respond to requests for specific information on perinatal HIV statistics.
Vanessa Rojas, a family medicine doctor and HIV specialist at Childrens Diagnostic & Treatment Center in Fort Lauderdale, sees many patients living with the virus as a result of mother-to-child transmission, and in her case, she works with children who are transitioning into adulthood.
“The situation is often challenging and complex for the child. The reason for this is that living with HIV brings with it a lot of complex factors including, but not limited to, social stigma, mental illness and living with a chronic illness,” she explained.
In Florida, authorities are aware of the serious problem that perinatal HIV transmission has caused and there is local legislation – Targeted Outreach for Pregnant Women Act (TOPWA) – enacted in 1998 that seeks to provide help and care for high-risk mothers.
Dr. Rojas has many patients living with HIV as a result of mother-to-child transmission, and she repeats the same advice to all pregnant women with the virus whenever she is asked about the disease.
“Take your antiretrovirals daily. Doing so confers less than a 1% chance of transmitting HIV to the fetus. In addition, they themselves maintain viral load suppression and work to maintain long-term survival.”
Although cases of children under 13 with HIV have been dropping over the years in Florida, the rate remains high for the state and the nation as a whole.
Between 2015 and 2019 the percentage of HIV infection diagnosed in Black/African American children ranged from 55% to 61% nationwide.
In 2019 alone, they accounted for 57% of diagnoses of infection with the virus, according to the CDC. The percentage is similar in Florida, and a powerful reflection of the cost of the disparities the country is experiencing.
Social breakdown
With the outbreak of the coronavirus pandemic in 2020, the nation experienced a break in its routines without dispensation which additionally affected the way Sexually Transmitted Diseases (STDs) were spread and treated.
The latest CDC reports showed that Florida, with 4,584 new cases in 2019, leads the nation in national HIV infections followed by California (4,354) and Texas (4,302).
Preliminary data for 2020 (subject to a 12-month reporting delay) would again rank Florida as the territory with the most new HIV diagnoses nationwide, 3,569 in total, followed by California (3,270) and Texas (2,877), but at the same time would mean a 17% drop in infections understandable in the context of the coronavirus pandemic.
In 2018 Florida had ranked second in the nation with new cases, and although in 2016 the number infections reached 4,700, the national spike placed Florida in a “health risk area” for the federal government.
“I think people have a very relaxed view of HIV because of the access to medicine and it’s not uncommon to hear a lot of times that they’re not too worried about getting infected with the virus,” said Dr. Patria Rojas, a professor at Florida International University’s (FIU) Robert Stempel College of Public Health and Social Work.
Some 116,689 people with HIV were living in Florida in 2019, with an additional estimated 18,000 men and women carrying the virus but unaware of their status, according to figures from the Florida government’s HIV Epidemiology Plan.
That means that nearly 10% of the estimated 1.2 million people in the U.S. who have HIV reside in Florida, according to CDC data.
The latest update from the Florida Department of Health noted that between 2010 and 2019, the overall rates of HIV and AIDS diagnoses in the state decreased 14% and 48%, respectively.
In the last five years, the number of new cases of Human Immunodeficiency Virus (HIV) fell by 2% in Florida.
To the comfort of the authorities the decrease was 4% between 2018 and 2019 going from 4,765 to 4,584 diagnoses, respectively.
When compared to the national average, however, the data becomes worrying because the infection rate is still among the highest.
HIV alarms in Florida have never been off, and no less disturbing is the rise in infections from other STDs such as gonorrhea, chlamydia and syphilis over the past decade, leading the federal government in 2019 to admit that this reality “amounts to a public health crisis.”
From 2014 to 2018, the rates of reported cases of primary and secondary syphilis, congenital syphilis, gonorrhea, and chlamydia increased 71%, 185%, 63%, and 19%, respectively.
“Less than 20 years ago, gonorrhea rates in the U.S. were at historic lows, syphilis was near elimination, and advances in chlamydia diagnosis made it easier to detect infections. That progress has been lost, in part because of challenges to our public health system,” Raul Romaguera, acting director of the CDC’s Division of STD Prevention, wrote in April in a report on the case.
In April the CDC revealed that more than 2.5 million cases of chlamydia, gonorrhea and syphilis were reported in 2019, a record high for the sixth year in a row. What’s serious is that it’s young people between 15 and 19 who are being infected the most.
In that regard, Florida has some cards to show.
More than 34,000 youth ages 15-19 in the state were diagnosed in 2018 with a bacterial STD, for a rate of 2,859 cases per 100,000 population.
“To see reductions in STD and HIV rates among this age group, progress is needed to expand the delivery of comprehensive sexual health education in Florida’s schools,” the state’s HIV prevention report admitted.
Pandemic consequences
Because of the confinement and remote work that slowed the country’s social life in the early months of the coronavirus pandemic, during March and April 2020 STD cases dropped dramatically compared with the same period in 2019, the CDC said.
However, a resurgence of gonorrhea and syphilis infections the rest of the year suggested that STDs overall may have increased during 2020, although the data are not yet published, the agency cautioned.
“With the pandemic, the risks of HIV infection are expected to have increased because with the confinement, many women were forced to be with their partners and have unprotected sex with them, in addition to the increase in violence and alcohol use,” said Dr. Rojas, the university professor.
In the case of Florida reports from the local Department of Health show that between 2017 and 2019 gonorrhea, syphilis and chlamydia have not stopped rebounding as a classic pattern of sexual diseases.
Chlamydia infection was the most frequently reported bacterial disease in the United States in 2019, affecting men and women equally.
In women, it can cause problems in the uterus and birth defects in babies if not treated early. Antibiotics are the most common medicine.
Florida recorded 104,758 cases of chlamydia in 2018, when it had reported 100,018 in 2017, one of the highest spikes in the country that year, according to the CDC.
The Federal Government is implementing a National Strategic Plan 2021-2025 which it hopes will reduce the high rates of STDs being reported.
Last March the White House approved a $1.3 billion budget under the American Rescue Plan Act to strengthen the workforce of disease intervention specialists (DIS) who have been vital in treating STDs, HIV, emerging threats such as Ebola, Zika, as well as hepatitis outbreaks and clusters.
The expansion of STD express clinics across the country that allow testing and treatment without an appointment or a full clinical examination has been a vital tool in the national containment strategy, the reports say.
But now, “repurposing” the resources that were used to overcome the COVID-19 pandemic, local governments are turning to telemedicine to ensure access for the potentially infected to health care providers, particularly in rural areas where HIV and STD cases are critical.
Behind the evils
Florida has become a bastion of tourism and a temple of American nightlife with beaches, sun and parties. Over the years, Florida has become for many a lustful mix of natives and foreigners who cross paths without taking any risks beyond a furtive night out.

That funnel of the multicultural world where so many nationalities intersect at the mercy of tourism helps to understand, in part, why the Sunshine State has become a health risk for authorities who in 2020 saw syphilis, gonorrhea and chlamydia among the most common sexually transmitted diseases.
When it comes to tracking HIV among Florida’s communities, the picture is also devastating: it reveals how the virus has been hitting racial minorities, and in the case of this state, Latinos carry much of the problem with African Americans at the top of the list.
The crisis surrounding this virus and all that it represents historically for the nation since the first cases in 1981 has been most acute in southern states (Alabama, Florida, Georgia, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee, and Texas) because of spiraling economic inequality, systemic racism, and lack of access to health insurance.
That tends to explain the reasons why 51% of the cases in 2019 were in southern states.
In fact, between 2015 through 2019, the number and rate of people living with HIV increased in the Midwest, South, and West, while the Northeast remained stable.
The ITEMP Project worked with data provided directly by the CDC and the Florida Department of Health, and although some of the data do not agree on exact numbers, the databases allowed us to piece together a puzzle of state public health that has been little explored in the midst of the coronavirus pandemic.
With a statewide average infection rate of 23.7 cases per 100,000 population, Miami-Dade, Broward, Duval and Orange counties (the latter is home to the city of Orlando) have the highest incidence of new HIV infections.

The four of them have the largest population in Florida with a large immigrant and minority community, and receive the bulk of the 100 million tourists who come to the state each year. That’s five times the population of the peninsula.
With some 20.1 million people living in Florida, the population is very diverse, with 20% of residents of foreign origin.
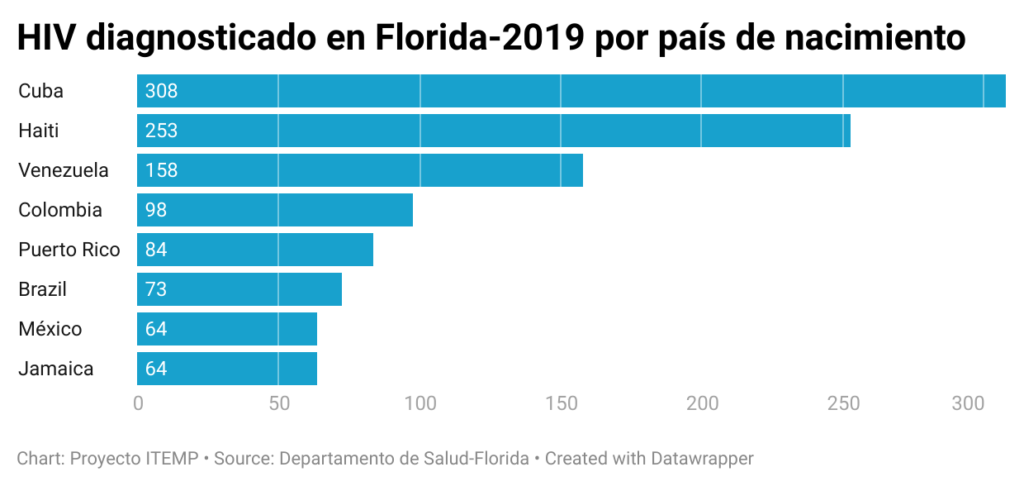
Although the majority of new HIV diagnoses in the state for 2019 were among those born in the country (61.1%), 38.9% of new cases were among those born outside the US.
The highest prevalence was among African-Americans, who received 38 percent of new HIV diagnoses and 49 percent of AIDS diagnoses even though they represent only 15 percent of adults in Florida, according to the state Department of Health.
HIV is the virus that causes the disease AIDS, so people who have the virus do not always have AIDS, which is why public health agencies are strict in differentiating each situation.
HIV is a potentially deadly virus that attacks the body’s immune system and leaves a person vulnerable to opportunistic infections.
No language distinction
Hispanics/Latinos in Florida were also disproportionately embodied for new HIV diagnoses in 2019, 36% of the total, compared to 24% among whites.
To get a dimension of this, according to the Census Bureau, the racial distribution among adults in Florida in 2019 was 55% White, 25% Hispanic/Latino, 15% African American, and 5% other races, which includes American Indian, Asian, or multiracial.
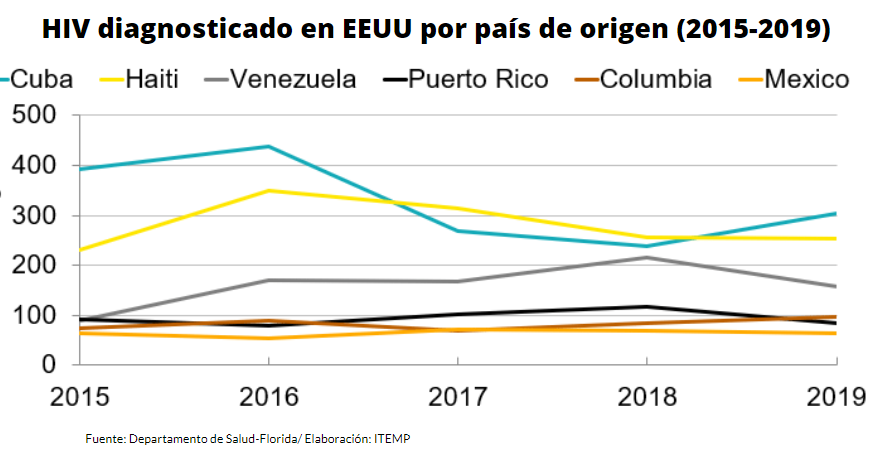
Hispanics born in Cuba (304), Haiti (253), Venezuela (158), Colombia (98), Puerto Rico (84) respectively, experienced the highest number of HIV diagnoses in 2019 in Florida, according to data from a state Department of Health presentation reviewed by ITEMP.
These immigrant communities, at the same time, are the largest in Florida, and the rate of contagion within them has been falling since the highest peak seen in 2016.
“This presents a need for increased training in cultural competency to ensure that education, prevention and health care services are delivered in a culturally and linguistically appropriate manner,” the state HIV health report acknowledged.
In fact, the number of new HIV diagnoses over the past five years in Florida declined in all race and ethnicity groups except two, Hispanics, which grew by 13% and by 125% among American Indians/Alaska Natives.
For Florida, the new HIV cases are disturbing, to be sure. But, at the same time, the data is encouraging because infections have been declining for the past 10 years.
The blue pill
Over the last decade (2010-2019), HIV and AIDS diagnosis rates in Florida dropped 14% and 48%, respectively, and public health experts link this decline to the progressive use of the pre-exposure prophylaxis (PrEP) pill known on the market as Truvada and Descovy. Or simply the “blue pill”.
“The effectiveness of PrEP is proven, and the fact that the federal and state governments are funding its use by providing subsidies to people who qualify is already a big help in joining the effort to avoid HIV infection just by taking a pill,” said a local leader in South Florida who is campaigning among the LGBTQ community to encourage them to enter the drug program.
“The incredible thing is that there are still people who are unaware of the existence of this method, our job is to reach them,” said the promoter, who asked not to reveal her name as she is not authorized by her organization to share comments.
As a daily pill, PrEP was approved by the FDA in 2012 and shown to be up to 90% effective in preventing the virus in people at higher risk for HIV in combination with safer sex practices.
Although male-to-male sexual contact remains the primary mode of exposure to HIV (75% of men diagnosed in 2019), the CDC recommends PrEP as a prevention tool regardless of a person’s sexual status.
PrEP prescribing is on the rise in Florida going from 8,367 people prescribed in 2017 to 33,458 in 2020, according to CDC indicators.
Unlike other states in the nation with a high incidence of HIV infection, use of the drug in Florida has grown to 26.7% of Floridians at high risk of contracting the virus last year, while New York is approaching 50% of prescribers with an estimated 34,321 people in 2020 taking a daily PrEP capsule.
A 2019 report by the National Medical Association following a study found that public health and education campaigns in South Florida promoting HIV prevention should focus on increasing awareness and utilization of PrEP among racial minorities in light of the fact that they are the most vulnerable group.
One of the key points of the new billion-dollar prevention budget that the White House approved is aimed at boosting the use of these drugs over the next five years.
In the particular case of Florida with the Department of Health’s goal of reducing the rate of new HIV transmission from 21.6 in 2019 to 5.4 by 2025, efforts will focus on increasing PrEP uptake, particularly for populations with higher rates of new HIV diagnoses.
“We have a population with enormous ignorance about how to avoid infection and how to talk about HIV prevention with their partners,” lamented Dr. Rojas of FIU.
When HIV began ravaging entire communities at a staggering rate across the United States in the 1980s, Americans faced an epidemic that stigmatized homosexuals and created a cycle of exclusion that was only narrowed over time, thanks to advancing research that showed that, regardless of sexual status, anyone was prone to infection.
Realistic goal
Walter Gomez’s ex-partner committed suicide in the summer of 2015 when the torment that consumed him as an HIV carrier destroyed his spirit and led him to take his own life.
He was 26 years old. One of the boys with whom he had sexual relations had infected him months before without knowing that he also carried the virus. Like the labyrinth that this disease becomes, Walter also became infected, but with him ended a long path of contagions that would have led to other men becoming ill.
“I think he committed suicide because of the panic of having infected me. He took some pills, I will never know, but I can imagine what he went through in those months. Today none of this would have happened, the antiretrovirals are stronger, there are pills to prevent infection,” Walter says on the phone from his home in Boston.
“There is more social acceptance among the LGBTQ community itself, and I think that, if there are contagions today, it’s because people really want to get sick. A pill can save you, not before,” he adds.
The US Government has set an ambitious goal of reducing all new HIV infections by 75% in 5 years and 90% by 2030.
Achieving this record requires a coordinated national effort in the hardest-hit states and 48 counties in the country that are hot spots for the virus, four of them in Florida.
The plan to reduce the scope of the virus is not a pipe dream 40 years after the first cases worldwide; tests for an eventual vaccine continue to expand in laboratories in many countries, although the use of condoms remains the infallible method to avoid contagion.
Dr. Rojas, the family medicine specialist, is hopeful that, unlike in the past, the numbers are showing a gradual reduction in infections and new cases, especially in someone as innocent and unworldly as a newborn.
“I believe these statistics provide hope for an end to the HIV epidemic. Mother-to-child transmission is an unfortunate outcome of the HIV epidemic, and knowing that the science is consistently strong gives great hope that one day we will no longer see mother-to-child transmission.